About HSP (Hereditary Spastic Paraplegia)
General Information
This material has been reviewed by Dr John Fink, M.D., SPF Medical Advisor. Please see the Glossary to help with medical terms.
Index:
- HSP Description by PM&R Knowledge
- What is HSP?
- National Organization of Rare Diseases Write Up on HSP
- What is (Apparently Sporadic) Spastic Paraplegia?
- What are the symptoms?
- Why are my symptoms different from others in my family?
- How does HSP cause symptoms?
- How severe will my symptoms get?
- How is HSP diagnosed?
- What genetic testing is available?
- What is the life expectancy?
- What is the treatment?
- What is the risk of getting HSP?
- What other conditions cause spastic paraplegia and weakness of muscles?
- SPG3A - Gene Review
- SPG4 - Gene Review
- SPG 5A - Pub Med
- SPG7 - Gene Review
- SPG8 - Gene Review
- SPG9A Autosomal Dominant
- SPG10 - Gene Review
- SPG11 - Gene Review
- SPG13 - American Journal of Human Genetics
- SPG15 - Genetics Home Reference
- An Overview of Developments in HSP Research
- CReATe Dr. Michael Benatar Univ of Miami, ALS & Related Disorders of PLS, HSP, PMA, & FTD
- You Tube Video about HSP
- Youtube Rebecca Schule PhD Webinar on HSP Oct 2020
- Adam Lawrence's HSP Blog
- Use of Continuous Intrathecal Baclofen in HSP
- How Reticulon 2 & Spastin Interact to Affect the Endoplasmic Reticulum
- Delving into the Complexity of HSP
- What Clinical Trials Can People With HSP Participate In?
- Download Video Explaining Gene Editing with CRISPR Technology
- Hereditary spastic paraplegia: Clinical-genetic characteristics and evolving molecular mechanisms
- Cellular pathways of hereditary spastic paraplegia
- SPG4: what is known and not known about the disease
- The endoplasmic reticulum: structure, function and response to cellular signaling
- A patient-derived stem cell model of hereditary spastic paraplegia with SPAST mutations
- Neurodegeneration and microtubule dynamics
- Structural basis of microtubule severing by the hereditary spastic paraplegia protein spastin
- The hereditary spastic paraplegia proteins NIPA1, spastin and spartin are inhibitors of mammalian BMP signalling
- Two Novel Mutations in Gene SPG4
- Mechanism of impaired microtubule-dependent peroxisome trafficking and oxidative stress in SPAST-mutated cells from patients with Hereditary Spastic Paraplegia
- Hereditary Spastic Paraplegia: Clinicogenetic Lessons from 608 Patients
- Every Reason to Hope - Understanding the Current State of HSP Research
- Study details defects in neurons associated with hereditary spastic paraplegia
- Hereditary spastic paraplegia proteins REEP1, spastin, and atlastin-1 coordinate microtubule interactions with the tubular ER network
- A Good Introduction to What CRISPR Is
- Audio Neurology Now interview with Dr. Craig Blackstone on What is HSP?
- An Overview Article About High-Arched Feet
- Selective dorsal rhizotomy for hereditary spastic paraparesis in children.
- Hereditary spastic paraplegia from 1880 to 2017: an historical review
- Q&A with Allen Bernard & Dr. Craig Blackstone, M.D. , Ph.D about HSP in March 2018
- Perspectives on the Genomics of HSP Beyond Mendelian Inheritance
- Recent advances in understanding hereditary spastic paraplegias and emerging therapies March 2021
-
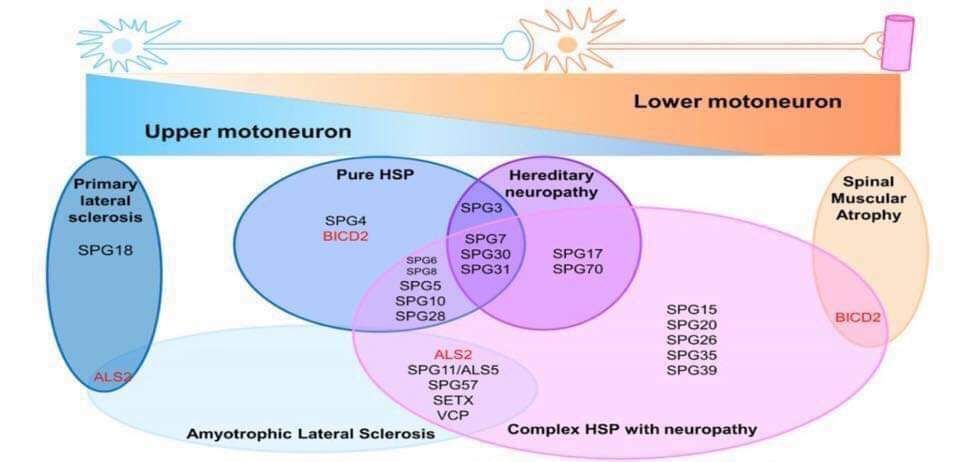
Hereditary Spastic Paraplegia (HSP) is a group of rare, inherited neurological disorders. Their primary symptoms are progressive spasticity and weakness of the leg and hip muscles. Researchers estimate that some 90 different types of HSP exist; the genetic causes are known for about fifty. The HSP incidence rate in the United States is about 20,000 people. The condition is characterized by insidiously progressive lower extremity weakness and spasticity. HSP is classified as uncomplicated or pure if neurological impairment is limited to the lower body. HSP is classified as complicated or complex if other systems are involved or if there are other neurological findings such as seizures, dementia, amyotrophy, extrapyramidal disturbance, or peripheral neuropathy in the absence of other disorders such as diabetes mellitus. Many different names are used for HSP. The most common are Hereditary Spastic Paraplegia (or Paraparesis), Familial Spastic Paraparesis (or Paraplegia), and Strümpell-Lorrain Disease. Others are Spastic Paraplegia, Hereditary Charcot-Disease, Spastic Spinal Paralysis, Diplegia Spinalis Progressiva, French Settlement Disease, Troyer syndrome, and Silver syndrome. The disorder was first identified in the late 1800s by A. Strümpell, a neurologist in Heidelberg, Germany. He observed two brothers and their father, all of whom had gait disorders and spasticity in their legs. After the death of the brothers, Strümpell showed through autopsy the degeneration of the nerve fibers leading through the spinal cord. HSP was originally named after Strümpell, and later after two Frenchmen, Lorrain and Charcot, who provided more information. Here’s an Overview Summary Chart.
-
Many individuals with all the signs and symptoms of HSP do not appear to have similarly affected family members. Without proof of a hereditary link, some neurologists call the condition Spastic Paraplegia or Apparently Sporadic Spastic Paraplegia. Other clinicians may diagnosis the same condition as Primary Lateral Sclerosis (PLS), which mimics HSP in how it affects the lower body. However, current researcher indicates that PLS eventually affects the arms and speech and swallowing muscles as well as the leg muscles. There are many reasons why someone with HSP may not have a family history. Recessive and x-linked forms skip generations, which means the disorder may pass silently for generations and then suddenly appear. In addition, the age of onset, progression rate and severity vary widely so that the disease could have gone undiagnosed in previous generations or an affected individual may have died before symptom onset. Mistaken parentage or new genetic mutations are also possible. Please see Heredity and Genetics for more information on this and genetic testing.
-
The hallmark of HSP is progressive difficulty walking due to increasingly weak and stiff (spastic) muscles. Symptoms appear in most people between the second and fourth decade of life, but they can start at any age. Initial symptoms are typically difficulty with balance, stubbing the toe or stumbling. Changes begin so gradually that other people often notice the change first. As the disease progresses, canes, walkers and eventually wheelchairs may become needed, although some people never require assistive devices. Other common symptoms of HSP are urinary urgency and frequency, hyperactive reflexes, difficulty with balance, clonus, Babinski’s sign, diminished vibration sense in the feet, muscle spasms, and congenital foot problems such as pes cavus (high arched foot). Some people may experience problems with their arms or fine motor control of their fingers but for most people, this is not significant. Most people with HSP have uncomplicated HSP. There are also rare, complicated forms, which have additional symptoms, such as peripheral neuropathy, ichtyosis (a skin disorder) epilepsy, ataxia, optic neuropathy, retinopathy, dementia, mental retardation, deafness, or problems with speech, swallowing or breathing. These symptoms may have other causes though, unrelated to HSP. For example, someone with uncomplicated HSP may have peripheral neuropathy caused by diabetes.
-
As noted above, the severity of symptoms and age of onset can vary widely, even within the same family. One reason is that HSP is a group of genetically different disorders, not a single disorder. Some differences may be due to genetic mutations. A child may show symptoms before a parent and it’s possible for some family members to have very mild symptoms while others have more severe symptoms. This may be due to other genes, environment, nutrition, general health, or factors not yet understood. In some families, symptoms tend to start at younger ages with each generation. Although rare, HSP sometimes shows “incomplete penetrance”. This means that occasionally, an individual may have the gene mutation, but for unknown reasons never develop symptoms of HSP. Such individuals can still pass HSP to their children.
-
HSP is caused by degeneration of the upper motor neurons in the brain and spinal cord. Upper motor neurons control voluntary movement. The cell bodies of these neurons are located in the motor cortex area of the brain. They have long, hair-like processes called axons that travel to the brainstem and down the spinal cord. Axons relay the messages to move to lower motor neurons that are located all along the brainstem and spinal cord. Lower motor neurons then carry the messages out to the muscles. Click on the diagram at right to see how upper motor neurons connect to lower motor neurons that innervate leg muscles. When upper motor neurons degenerate, the correct messages cannot reach the lower motor neurons, and the lower motor neurons cannot transmit the correct messages to the muscles. As the degeneration continues, spasticity and weakness increase. The legs are affected because degeneration occurs primarily at the ends of the longest nerves in the spinal cord, which control the legs. In some cases, the upper body can be minimally affected as well, leading to problems with the arms or speech and swallowing muscles.
-
There is no way to predict rate of progression or severity of symptoms. Generally, once symptoms begin, progression continues slowly throughout life. For some childhood-onset forms, symptoms become apparent, gradually worsen during childhood, and then stabilize after adolescence. HSP rarely results in complete loss of lower limb mobility.
-
HSP is diagnosed via a careful clinical examination, by excluding other disorders that cause spasticity and weakness in the legs, and by an observation period to see if other symptoms develop that indicate another condition, such as PLS. Disorders that can be ruled out with testing are ALS, tropical spastic paraparesis (TSP), vitamin deficiencies (B12 or E), thoracic spine herniated disks, and spinal cord tumors or injuries and multiple sclerosis. HSP can resemble cerebral palsy, however, HSP is degenerative and thereby causes increasing spasticity and weakness of the muscles. Two other disorders with spastic paraplegia symptoms termed Lathyrism and Konzo are caused by toxins in the plants Lathyrus sativus and cassava. HSP is hereditary, and examining family history is important in diagnosing HSP. However, many individuals with all the signs and symptoms of HSP do not have a family history. See (Apparently Sporadic) Spastic Paraparesis.
-
Invitae Corp Hereditary Spastic Paraplegia (HSP) panel has 78 genes on it, and those genes are known to cause 67 different types of HSP or related disorders.
Athena Diagnostics HSP panel, Comprehensive Evaluation has 24 genes on it, and the associated disorders are not specified. Athena also offers 9 related sub-panels for different HSP presentations (recessive, dominant, common, etc).
Both companies let you order any gene on the panel on its own.
As more genes are discovered, it is hopeful that such information will lead to greater availability of testing. Genetic counselors can be found at many major medical centers or by contacting the National Society of Genetic Counselors at (610) 872-7608. Gene tests can be used for prenatal testing.
-
Life expectancy is normal. However, complications arising from falls or immobility caused by the symptoms of HSP may inadvertently shorten a person’s life.
-
No treatments are currently available to prevent, stop, or reverse HSP. Treatment is focused on symptom relief, such as medication to reduce spasticity; physical therapy and exercise to help maintain flexibility, strength, and range of motion; assistive devices and communications aids; supportive therapy and other modalities. See treatment and therapies for additional detailed information.
-
There are some seventy different forms of HSP, with three different modes of inheritance: autosomal dominant, autosomal recessive and X-linked. Each mode has a different risk factor, which ranges from almost none to 50%. See Heredity and Genetics for additional detailed information.
-
Muscle spasticity and weakness can also be caused by other conditions including (but not limited to) Tropical Spastic Paraparesis and conditions called Lathyrism and Konzo caused by toxins in the plants lathyrus sativus and cassava that also cause muscle spasticity and weakness.
-
The Spastic Paraplegia Foundation has gained permission from The Russian Academy of Sciences to provide this study to our membership, free of charge.
-
Many people find the tightness in their muscles worsens when they are angry, stressed, or upset. This may make it more difficult to walk and speak. It is unknown exactly how emotions affect muscle tone, but it may involve adrenalin levels. Most people also report increased stiffness in cold weather.
-
Periods of feeling down about having HSP are normal and expected. It is not uncommon for people to also experience periods of clinical depression.
-
Memory disturbance has been reported in some individuals with HSP due to spastin gene mutations. In general, it was mild. Before attributing memory disturbance to HSP, it is important to consider other causes: stress, anxiety, depression, lack of sleep, medications (including Baclofen), other health conditions including vitamin B12 deficiency. If memory disturbance is significant, a cause of concern, or worsening, it would be important to discuss this with your primary physician and neurologist.
-
Yes. Here are a few examples:
-High arched feet (pes cavus). High arches occur because there is more weakness in the foot muscles that extend the foot backward and flatten the arch than in the muscles that flex the foot downward.
-Shortened Achilles tendons. Achilles tendons are often short, and generally shorten further as HSP progresses.
-Jumping feet (clonus). Clonus is an uncontrollable, repetitive jerking of muscles that makes the foot jump rapidly up and down. It occurs when the foot is in a position that causes a disruption of the signals from the brain, leading to an automatic stretch reflex.
-Hammer toes or bunions. These may occur due to imbalances in the strength and tone of muscles that maintain proper alignment of joints in the feet.
-Cold feet and/or foot swelling. This is most likely caused by poor circulation. Normally, muscle contractions in the legs help pump blood from the legs back to the heart. If the muscles are weakened, or if the person is relatively inactive, the blood flow from the legs may be decreased, and fluids may accumulate. This can cause swelling, or a sensation of “cold feet”. -
Some people may experience problems with their arms or fine motor control of their fingers. The degeneration in nerves that supply the arms is mild compared to that which occurs in the nerves that supply the legs. For most people, this is not significant.
-
The short answer appears to be “yes”, although it is important to remember that sexual desire and/or function can be affected by many other factors such as age, stress, depression, fatigue, medical disorders or medications. Some people report that stiffness, spasms and cramps that are part of HSP may either inhibit (or intensify) orgasm, or that orgasm may bring on leg stiffness, spasms or clonus. Stiffness of the legs or arms may cause difficulty using certain positions for intercourse. Baclofen, particularly intrathecal baclofen, has been linked to anorgasmia (type of sexual dysfunction in which a person cannot achieve orgasm, even with adequate stimulation) after a number of years of use.
-
No. The group of disorders known as Ataxias (such as Friedreichs Ataxia) are spino-cerebellar disorders in which there is a disturbance either in the part of the brain known as the cerebellum or in the connections to it. HSP does not involve the cerebellum. Ataxias can be hereditary or sporadic. The term “ataxia” means without coordination, and can also refer to a symptom in which there is a lack of muscle control resulting in a jerky or unsteady movement. People with HSP may have in coordination as a symptom. This does not mean they have Ataxia.
-
HSP cannot be passed to others through donation of blood. There is no medical reason why a person with HSP cannot donate blood.
-
In the late 1800’s, A. Strümpell, a neurologist in Heidelberg Germany, described this disorder. He observed two brothers and their father, who had gait disorders and spasticity in their legs. After the death of the brothers, Strümpell was able to show through autopsy the degeneration of the nerve fibers leading through the spinal cord. The disorder was originally named after Strümpell, and after two Frenchmen who later provided more information about the disorder, Lorrain and Charcot.
-
There is no evidence that HSP is more prevalent in one ethnic group than another.
Our Impact since our inception...
-
Dollars Raised
Over 12,000,000 dollars for research!