About PLS (Primary Lateral Sclerosis)
A Work in Progress
Neurologist & Psychiatrist
Dr. Deborah Warden
Deborah developed a mysterious neurologic illness, later to be revealed as PLS, while working with military blast TBI patients.
Visit her website to find out more about her.
Listen to her speak in a July 2025 speech using a voice clone recently made by Eleven Labs. You can compare the voice clone to the beginning of the video to see how similar the voice clone is to her original voice HERE
The disorder usually begins in the legs but can begin in the upper body or bulbar (speech and swallowing) muscles. The age of onset is generally between 35 and 66 years of age.
General Information
This material has been reviewed by Dr John Fink, M.D., SPF Medical Advisor. Please see the Glossary to help with medical terms.
Index:
- What is PLS?
- What are the symptoms?
- How does PLS cause my symptoms?
- How severe will my symptoms get?
- How is PLS diagnosed?
- How is PLS different from ALS?
- What is the treatment?
- What is the life expectancy?
- What other conditions cause spasticity and weakness of muscles?
- Primary Lateral Sclerosis Natural History Study - This study was funded by the Spastic Paraplegia Foundation, and a paper was published in September 2025.
- PLS - A Study by PLOS One
- Help for Speech, Swallowing & Salivation Problems in ALS
- Mayo Clinic Definition of PLS
- What Clinical Trials Can People with PLS Participate in?
-
Primary Lateral Sclerosis (PLS) is a group of rare, degenerative, neurological disorders. They are sporadic, meaning there is no clear familial link, although there are hereditary forms of PLS. PLS is caused primarily by degeneration of the upper motor neurons in the brain and spinal cord, which results in increasing spasticity and weakness of voluntary muscles. It is often referred to as a benign variant of Amyotrophic Lateral Sclerosis (ALS, Lou Gehrig’s disease).
The primary difference between the two is that in PLS the spinal motor neurons or lower motor neurons stay intact. Thus, there is no muscle wasting (amyotrophy), which is the symptom that ultimately causes fatal complications in ALS.
The disorder usually begins in the legs but can begin in the upper body or bulbar (speech and swallowing) muscles. The age of onset is generally between 35 and 66 years of age, with a median age of 50. The incidence rate for PLS is difficult to determine. One study puts it at 500 individuals in the United States. However, many researchers feel this is inaccurate, and that the actual incidence rate is closer to 2000. The issue is further complicated by the fact that researchers also believe a good portion of those initially diagnosed with PLS may have ALS or HSP.
PLS was first identified in France in the 1850s by Dr. Jean-Martin Charcot. During his landmark analyses of ALS patients, Dr. Charcot encountered a woman with severe spasticity and limb contractures but no muscle wasting. After she died in 1856, the autopsy revealed extensive scarring in the lateral columns of her spinal columns or primary lateral sclerosis.
Here’s an Overview Summary Chart. -
The hallmark of PLS is progressive weakness and spasticity of voluntary muscles. The first symptoms are often tripping or difficulty lifting the legs. Other people may be the first to notice a change in the affected person’s gait. Occasionally, speaking (dysarthria) and swallowing (dysphagia) difficulties, or arm weakness are the first symptoms. Speech problems can begin with hoarseness, a reduced rate of speaking, excessive clearing of the throat, or slurred speech when a person is tired. In some cases, speech becomes so slurred that others cannot understand it. Drooling can be a problem as well due to weakened bulbar muscles.
Wherever symptoms originate, the legs, arms, hands, and speech and swallowing muscles will all eventually be affected. In time, assistive devices are needed, such as canes, walkers, or wheelchairs. Speech therapy and communication aids may become necessary as well. Many people report painful muscle spasms and other pain. Other common symptoms are hyperactive reflexes and Babinkski’s sign. Emotional lability is often reported as well.
-
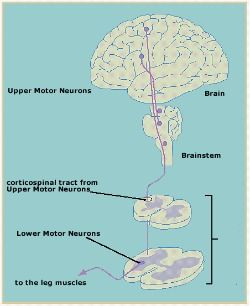
As noted above, PLS is caused by degeneration of the upper motor neurons in the brain and spinal cord. Upper motor neurons control voluntary movement.
The cell bodies of these neurons are located in the motor cortex area of the brain. They have long, hair-like processes called axons that travel to the brainstem and down the spinal cord. Axons relay the messages to move to lower motor neurons that are located all along the brainstem and spinal cord. Lower motor neurons then carry the messages out to the muscles. Click on the diagram at right to see how upper motor neurons connect to lower motor neurons that innervate leg muscles.
When upper motor neurons degenerate, impulses cannot adequately reach the lower motor neurons and the lower motor neurons cannot deliver the proper message to the corresponding muscle. The result is muscle weakness and spasticity. As the degeneration progresses, symptoms increase.
In PLS, the degenerative process impacts the length of the spinal cord, thus affecting the legs, arms and speech and swallowing muscles. For most patients, the process begins in the legs and then travels up the spinal cord. In some people, the process begins in the brainstem, affecting the speech and swallowing muscles first, and then descends down the spinal cord.
-
The rate at which symptoms will progress and how severe they will become is impossible to predict. In general, the course is a slowly progressive one. Some individuals report periods of acceleration, while others have long plateaus where progression appears to stop.
Researchers believe it can take several years for all parts of the body to become affected. An individual’s genes, environment, nutrition, general health, and other factors may influence the rate of progression and severity of the disease.
-
PLS is diagnosed via a careful clinical examination, by excluding other disorders that cause progressive spasticity and weakness, and by an extended observation period. Tests include a complete neurological examination, blood work, an MRI of the brain and spine, motor and sensory nerve conduction studies, and cerebrospinal fluid analysis. Some of these tests are repeated periodically. Conditions that can be ruled out with testing are tropical spastic paraparesis (TSP), vitamin deficiencies (B12 or E), thoracic spine herniated disks, spinal cord tumors or injury, cerebral palsy, and multiple sclerosis.
Some that may not be ruled out initially include forms of Amyotrophic Lateral Sclerosis where there is no or minimal lower motor neuron involvement, and Hereditary Spastic Paraplegia where there is just lower body and no lower motor neuron involvement. Within a few years, it is evident whether the disorder is actually ALS. Continued observation of clinical symptoms helps differentiate PLS from HSP.
-
ALS is a rapidly progressive, fatal, neuromuscular disease. As noted above, ALS is caused by degeneration of the lower motor neurons (the nerves that travel from the brainstem and spinal cord out to the muscles), which results in muscle wasting, as well as the upper motor neurons. Fifty-percent of ALS patients die from respiratory failure or pneumonia within three to five years of diagnosis.
However, there are some slowly progressing forms of ALS that are difficult to distinguish from PLS. In fact, up to 10% of ALS patients survive more than ten years. In addition, improved medical care is resulting in longer and more productive lives for all ALS patients.
-
No treatments are currently available to prevent, stop, or reverse PLS. Treatment is focused on symptom relief, such as medication to reduce spasticity; physical therapy and exercise to help maintain flexibility, strength, and range of motion; assistive devices and communications aids; and supportive therapy and other modalities. See treatment and therapies for additional detail.
-
Life expectancy is normal. However, complications from falls or immobility may inadvertently shorten a person’s life.
-
Muscle spasticity and weakness can also be caused by other conditions including (but not limited to) Primary Lateral Sclerosis, spinal cord injury or tumors, cerebral palsy, multiple sclerosis, amyotrophic lateral sclerosis, vitamin absorption, and thoracic spine herniated disks.
There is a virus-caused disease called Lathyhrus Tropical Spasticrism and Konzo caused by toxins in the plants lathyrus sativus and cassava that also cause muscle spasticity and weakness.
-
Many people find the tightness in their muscles worsens when they are angry, stressed, or upset. This may make it more difficult to walk and speak. It is unknown exactly how emotions affect muscle tone, but it may involve adrenalin levels. Most people also report increased stiffness in cold weather.
-
Periods of feeling down about having PLS are normal and expected. It is not uncommon for people to also experience periods of clinical depression.
-
The short answer appears to be “yes”, although it is important to remember that sexual desire and/or function can be affected by many other factors such as older age, stress, depression, fatigue, medical disorders or medications.
Some people report that stiffness, spasms and cramps that are part of PLS may either inhibit (or intensify) orgasm, or that orgasm may bring on leg stiffness, spasms or clonus. Stiffness of the legs or arms may cause difficulty using certain positions for intercourse.
-
Patients with PLS may donate blood. PLS cannot be passed to others through blood.
-
There is no evidence that PLS is more prevalent in one ethnic group than another.
Our Impact since our inception...
-
Dollars Raised
Over 12,000,000 dollars for research!